Two PhD candidates within the UQ School of Pharmacy have put their studies on hold and returned to full-time practice to help ease pressure on the workforce during the COVID-19 pandemic.
Ms Ellen Janke is working in a Queensland Health pharmacy department, while Ms Silke Chalmers has returned to community pharmacy.
They took time out of their busy work schedules to answer questions about their current experiences and the motivation behind them.
What role are you playing in the UQ School of Pharmacy’s response to the COVID-19 crisis?
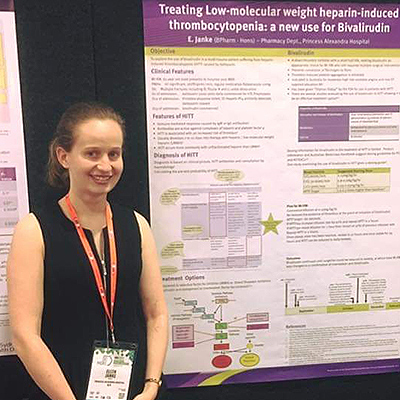
Ellen: In response to increased demand on the health service during the COVID-19 pandemic, I have chosen to take leave from my PhD studies and increase my hours within my role in Queensland Health.
Silke: I have suspended my HDR (Higher Degree Research) candidature for three months in order to provide assistance to the health workforce by returning to work as a community pharmacist.
What does your role entail?
Ellen: My job includes helping patients to manage their medications in the community and therefore avoid hospital admissions where possible. This, in turn, relieves pressure on our hospital system. There has been an increased use of telehealth (video conferencing, etc) to minimise face-to-face contact with patients and therefore, reduce the risk of spreading COVID-19.
The pharmacy department within Queensland Health has become directly responsible for monitoring of the use of alcohol-based hand sanitiser and disinfectant wipes to minimise misappropriate use of these resources. This has further increased our workload.
I have also taken on some shifts in the rehabilitation wards. We have increased the number of beds within our wards so that the hospitals can transfer patients to us, thus freeing up beds for patients infected with COVID-19.
Silke: My role in community pharmacy involves providing primary healthcare, medication supply and advice to the general community.
Community pharmacists are currently facing an unprecedented time of high demand and rapid change due to the pandemic. There is now increased flexibility for dispensing, which has coincided with an increased demand for medication supply/delivery services, and medication management services in the community.
Community pharmacists are also frontline in coordinating mass vaccination of the community to reduce the prevalence of influenza and to prevent flu co-morbidities.
What barriers/challenges have you come up against?
Ellen: Fear of COVID-19 is understandably limiting the amount of contact community-dwelling patients wish to have with healthcare workers. This can sometimes make it difficult to perform a complete and accurate medication history and pharmacy assessment of the patient as sometimes this requires access to the patient's home. The technology infrastructure fails sometimes, which makes it difficult to participate in telehealth consults with patients.
Clinicians who usually work within the Community and Oral Health Department of Queensland Health have been called to help out at the acute hospitals which leaves us short-staffed, and there is often frustration from fellow healthcare workers regarding the difficulty of accessing hand sanitiser.
Silke: Working directly with the public, our challenges have been associated with ensuring staff and patient safety through upgraded protective and sanitising protocols, as well as identifying our regular patients with high vulnerability to coordinate medication supply options which allow the patient to stay home.
We are also experiencing increased workloads as a result of the shift to telehealth consultations. Patients who are conscious of reducing strain on general practitioners are increasingly presenting to community pharmacies for initial advice. Additionally, dispensing from digital or faxed prescriptions currently increases our administrative work.
Finally, pharmacists are undergoing increasing pressure from a stressed and anxious public, which has unfortunately resulted in some pharmacy staff being abused over issues out of their control, including medication shortages.
Do you envisage more changes to your role, given the current environment?
Ellen: As the COVID-19 situation continues to develop, I might be needed to help out in other services within the Community and Oral Health Department of Queensland Health or I may be re-deployed to an acute hospital.
Silke: There are recommendations from the federal Health Minister to provide further flexibility for dispensing, which will assist pharmacists facing issues with medication shortages. Furthermore, laws around changed telehealth dispensing, when enacted in Queensland, may help to ease some of our aforementioned administrative workload.
During this time, I have been consistently impressed by the collaboration within the health care workforce, both inside and across disciplines. The increased interprofessional support I have experienced during this time has been a testament to the ingenuity, compassion, and resilience of healthcare workers.
Other staff and students from the UQ School of Pharmacy have stepped up to ease the pressure on the health workforce during the COVID-19 pandemic. read their story



